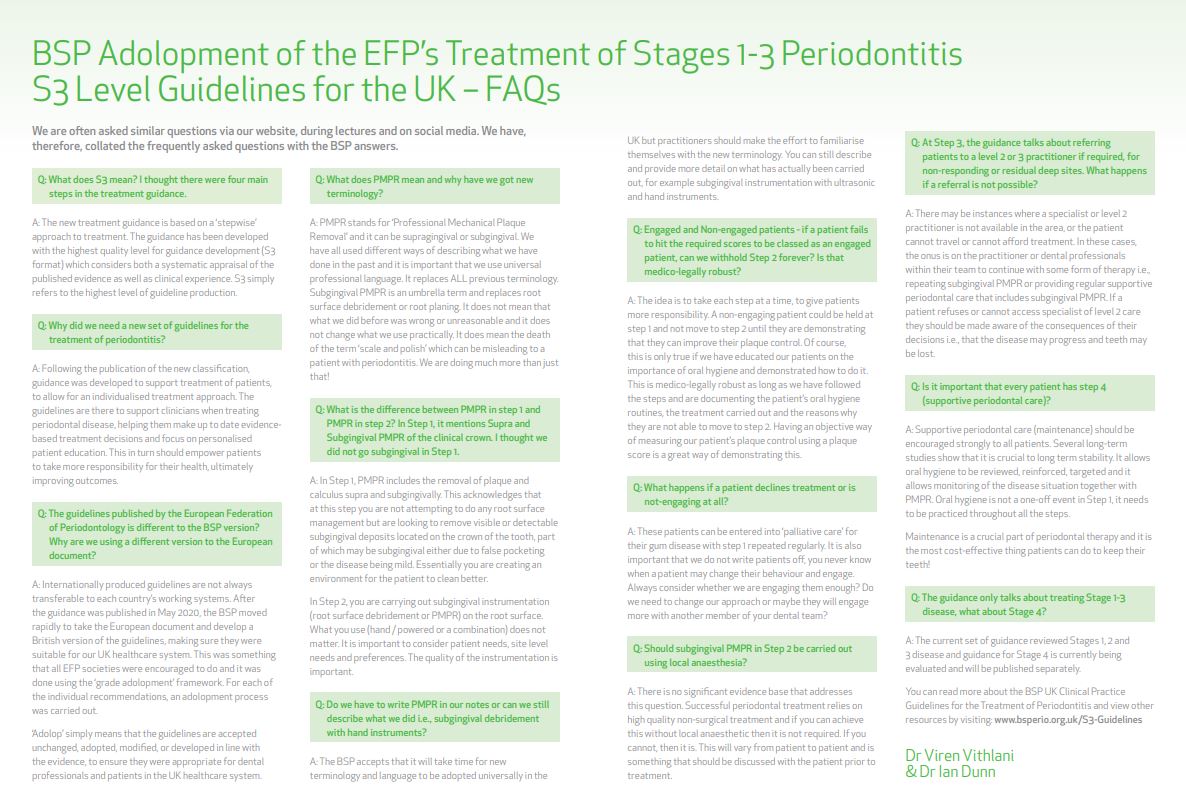
S3 Treatment Guidelines for Periodontitis
We are often asked similar questions via our website, during lectures and on social media. Dr Viren Vithlani & Dr Ian Dunn have, therefore, collated the frequently asked questions with the BSP answers:
Q: What does S3 mean? I thought there were four main steps in the treatment guidance.
A: The new treatment guidance is based on a ‘stepwise’ approach to treatment. The guidance has been developed with the highest quality level for guidance development (S3 format) which considers both a systematic appraisal of the published evidence as well as clinical experience. S3 simply refers to the highest level of guideline production.
Q: Why did we need a new set of guidelines for the treatment of periodontitis?
A: Following the publication of the new classification, guidance was developed to support treatment of patients, to allow for an individualised treatment approach. The guidelines are there to support clinicians when treating periodontal disease, helping them make up to date evidence based treatment decisions and focus on personalised patient education. This in turn should empower patients to take more responsibility for their health, ultimately improving outcomes.
Q: The guidelines published by the European Federation of Periodontology are different to the BSP version? Why are we using a different version to the European document?
A: Internationally produced guidelines are not always transferable to each country’s working systems. After the guidance was published in May 2020, the BSP moved rapidly to take the European document and develop a British version of the guidelines, making sure they were suitable for our UK healthcare system. This was something that all EFP societies were encouraged to do and it was done using the ‘grade adolopment’ framework. For each of the individual recommendations, an adolopment process was carried out. ‘Adolop’ simply means that the guidelines are accepted unchanged, adopted, modified, or developed in line with the evidence, to ensure they were appropriate for dental professionals and patients in the UK healthcare system.
Q: What does PMPR mean and why have we got new terminology?
A: PMPR stands for ‘Professional Mechanical Plaque Removal’ and it can be supragingival or subgingival. We have all used different ways of describing what we have done in the past and it is important that we use universal professional language. It replaces ALL previous terminology. Subgingival PMPR is an umbrella term and replaces root surface debridement or root planing. It does not mean that what we did before was wrong or unreasonable and it does not change what we use practically. It does mean the death of the term ‘scale and polish’ which can be misleading to a patient with periodontitis. We are doing much more than just that!
Q: What is the difference between PMPR in step 1 and PMPR in step 2? In Step 1, it mentions Supra and Subgingival PMPR of the clinical crown. I thought we did not go subgingival in Step 1.
A: In Step 1, PMPR includes the removal of plaque and calculus supra and subgingivally. This acknowledges that at this step you are not attempting to do any root surface management but are looking to remove visible or detectable subgingival deposits located on the crown of the tooth, part of which may be subgingival either due to false pocketing or the disease being mild. Essentially you are creating an environment for the patient to clean better. In Step 2, you are carrying out subgingival instrumentation (root surface debridement or PMPR) on the root surface. What you use (hand / powered or a combination) does not matter. It is important to consider patient needs, site level needs and preferences. The quality of the instrumentation is important.
Q: Do we have to write PMPR in our notes or can we still describe what we did i.e., subgingival debridement with hand instruments?
A: The BSP accepts that it will take time for new terminology and language to be adopted universally in the UK but practitioners should make the effort to familiarise themselves with the new terminology. You can still describe and provide more detail on what has actually been carried out, for example subgingival instrumentation with ultrasonic and hand instruments.
Q: Engaged and Non-engaged patients - if a patient fails to hit the required scores to be classed as an engaged patient, can we withhold Step 2 forever? Is that medico-legally robust?
A: The idea is to take each step at a time, to give patients more responsibility. A non-engaging patient could be held at step 1 and not move to step 2 until they are demonstrating that they can improve their plaque control. Of course, this is only true if we have educated our patients on the importance of oral hygiene and demonstrated how to do it. This is medico-legally robust as long as we have followed the steps and are documenting the patient’s oral hygiene routines, the treatment carried out and the reasons why they are not able to move to step 2. Having an objective way of measuring our patient’s plaque control using a plaque score is a great way of demonstrating this.
Q: What happens if a patient declines treatment or is not-engaging at all?
A: These patients can be entered into ‘palliative care’ for their gum disease with step 1 repeated regularly. It is also important that we do not write patients off, you never know when a patient may change their behaviour and engage. Always consider whether we are engaging them enough? Do we need to change our approach or maybe they will engage more with another member of your dental team?
Q: Should subgingival PMPR in Step 2 be carried out using local anaesthesia?
A: There is no significant evidence base that addresses this question. Successful periodontal treatment relies on high quality non-surgical treatment and if you can achieve this without local anaesthetic then it is not required. If you cannot, then it is. This will vary from patient to patient and is something that should be discussed with the patient prior to treatment.
Q: At Step 3, the guidance talks about referring patients to a level 2 or 3 practitioner if required, for non-responding or residual deep sites. What happens if a referral is not possible?
A: There may be instances where a specialist or level 2 practitioner is not available in the area, or the patient cannot travel or cannot afford treatment. In these cases, the onus is on the practitioner or dental professionals within their team to continue with some form of therapy i.e., repeating subgingival PMPR or providing regular supportive periodontal care that includes subgingival PMPR. If a patient refuses or cannot access specialist of level 2 care they should be made aware of the consequences of their decisions i.e., that the disease may progress and teeth may be lost.
Q: Is it important that every patient has step 4 (supportive periodontal care)?
A: Supportive periodontal care (maintenance) should be encouraged strongly to all patients. Several long-term studies show that it is crucial to long term stability. It allows oral hygiene to be reviewed, reinforced, targeted and it allows monitoring of the disease situation together with PMPR. Oral hygiene is not a one-off event in Step 1, it needs to be practiced throughout all the steps. Maintenance is a crucial part of periodontal therapy and it is the most cost-effective thing patients can do to keep their teeth!
Q: The guidance only talks about treating Stage 1-3 disease, what about Stage 4?
A: The current set of guidance reviewed Stages 1, 2 and 3 disease and guidance for Stage 4 is currently being evaluated and will be published separately. You can read more about the BSP UK Clinical Practice Guidelines for the Treatment of Periodontitis and view other resources by visiting: www.bsperio.org.uk/S3-Guidelines